IOPS®
Intra-Operative Positioning System
A New Way to Envision Endovascular Navigation
Centerline Biomedical’s Intra-Operative Positioning System (IOPS®) technology is an innovative, 3D GPS-like surgical navigation technology that improves endovascular procedure outcomes and reduces radiation exposure.
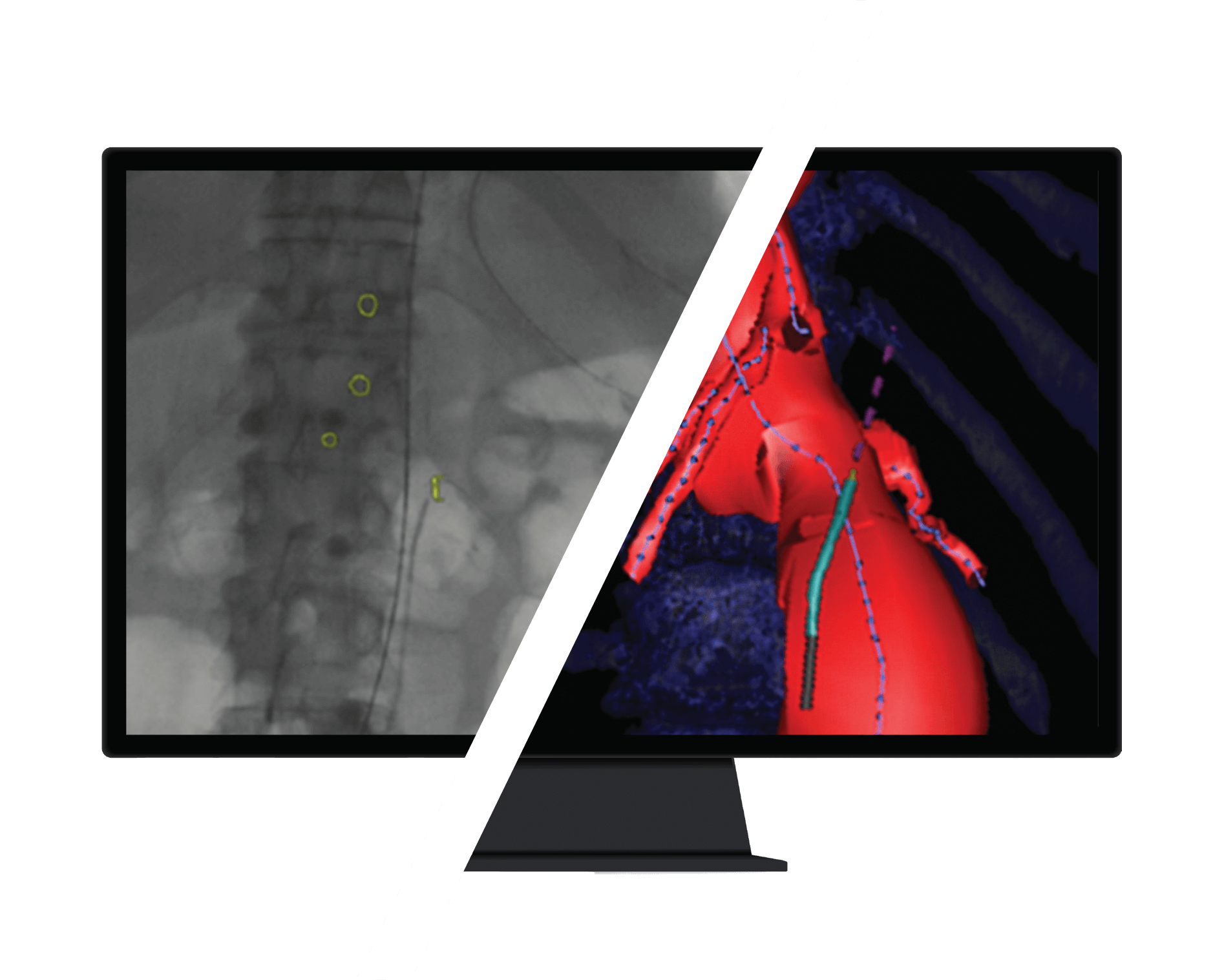
YESTERDAY
X-Ray Fluoroscopy
- Current “gold standard”
- Used in 4 million procedures per year
- Low-quality 2D Image Guidance
- Relies on harmful radiation and contrast dye
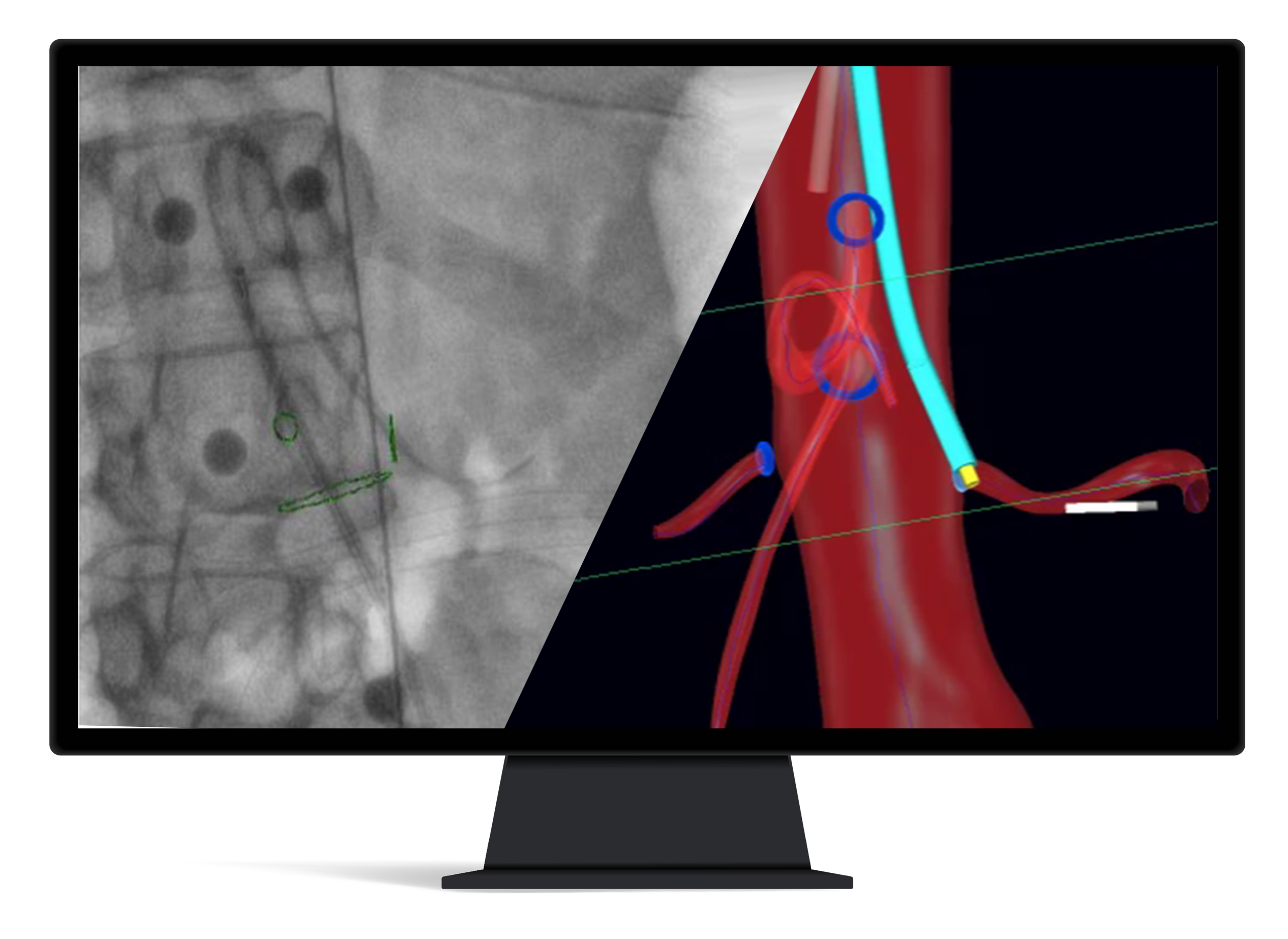
TODAY
IOPS® Navigation
- Interactive navigation with real-time positioning
- High-quality 3D Image Guidance
- Portable system
- Decrease radiation exposure
YESTERDAY
X-Ray Fluoroscopy
- Current “gold standard”
- Used in 4 million procedures per year
- Low-quality 2D Image Guidance
- Relies on harmful radiation and contrast dye
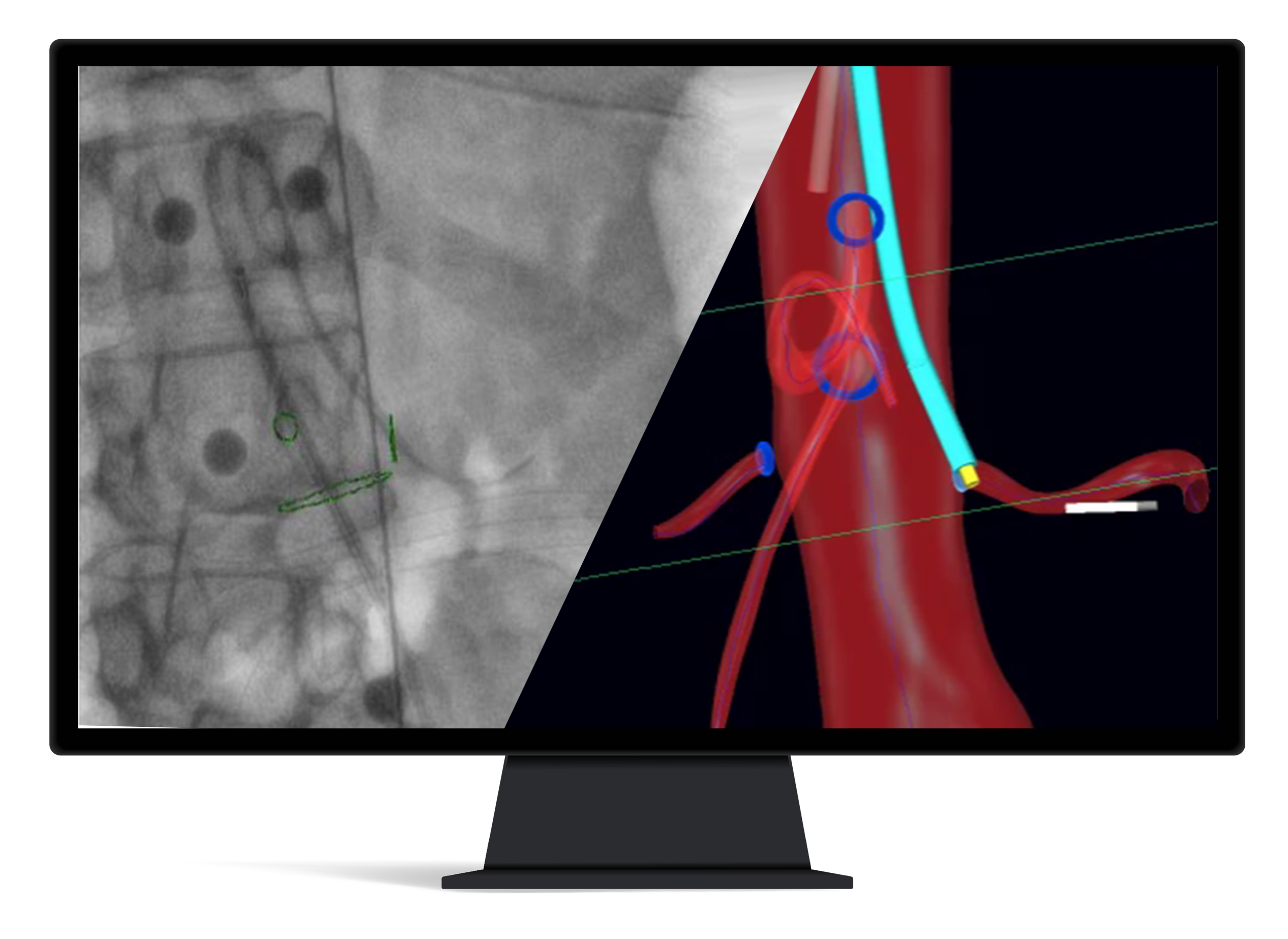
TODAY
IOPS® Navigation
- Interactive navigation with real-time positioning
- High-quality 3D Image Guidance
- Portable system
- Decrease radiation exposure
YESTERDAY
X-Ray Fluoroscopy
- Current “gold standard”
- Used in 4 million procedures per year
- Low-quality 2D Image Guidance
- Relies on harmful radiation and contrast dye
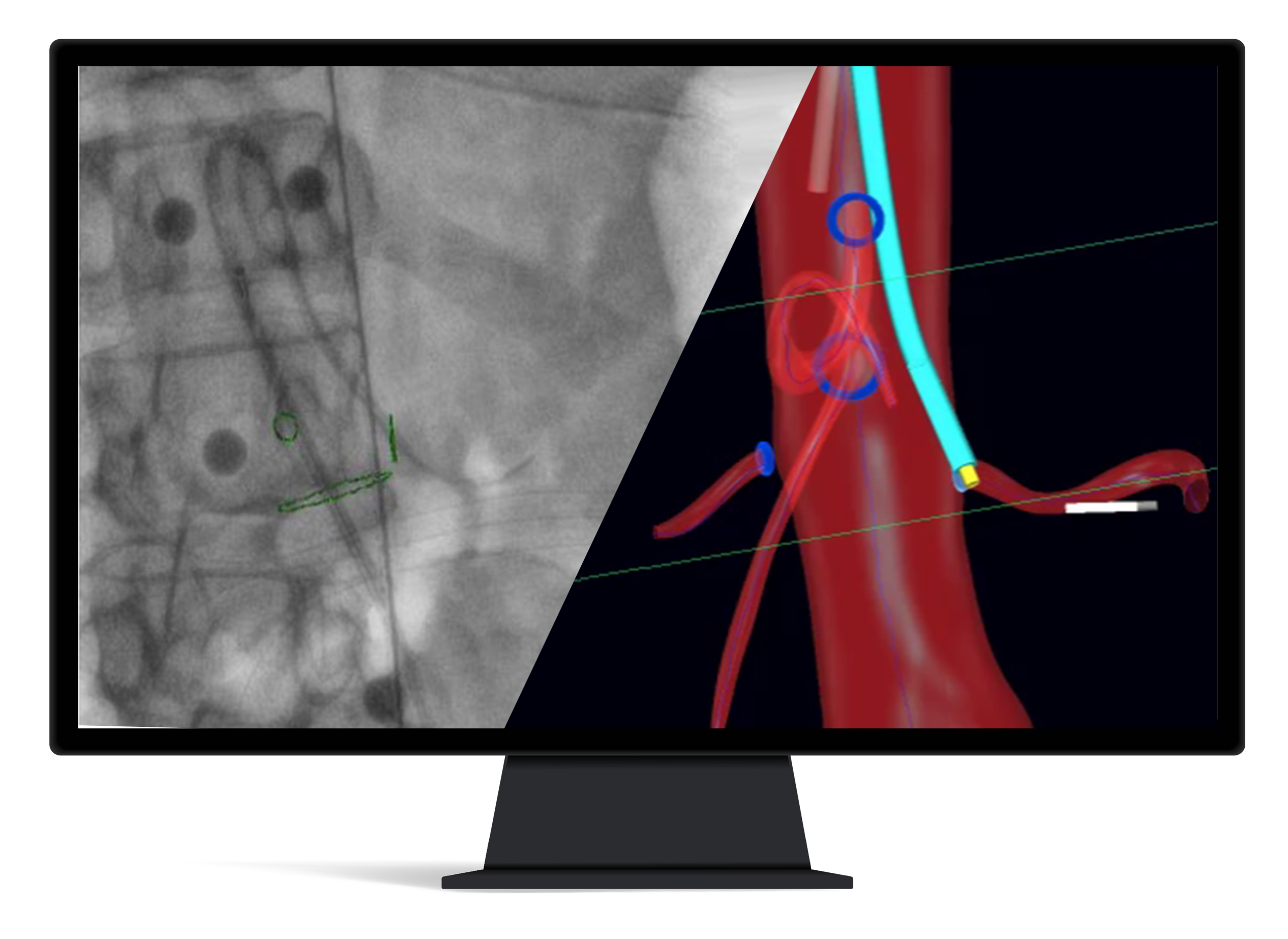
TODAY
IOPS® Navigation
- Interactive navigation with real-time positioning
- High-quality 3D Image Guidance
- Portable system
- Decrease radiation exposure
IOPS® ADVANTAGE
Time Reduction
A recent in vitro study found that, overall, the mean time necessary to cannulate a given vessel using 3D navigation was 53.4% of the time necessary using traditional 2D navigation, indicating a time savings of 46.6%
IOPS® ADVANTAGE
Improved Visualization Leads to Better Outcomes
Patient outcomes are improved as we reduce procedural times with better visualization, greater control, and real-time position navigation data.
IOPS® ADVANTAGE
Mitigate the Growing Risk of Radiation Exposure and Contrast Dye
As endovascular procedures become more complex, the risk of radiation exposure continues to increase.

%
Display significant posterior subcapsular lens changes, a precursor to cataracts 1
%
Of self-reported brain tumors in interventionalists originated on the left side of the head, the area closest to the radiation source 2
%
Incidence of spine issues after 21 years in practice, a result of wearing heavy radiation protection apparel 3

%
Of interventional cardiologists miss work due to orthopedic issues 4
1. Vano E, et al. Radiation-associated lens opacities in catheterization personnel: results of a survey and direct assessments. Journal of Vascular Interventional Radiology 2013;2: 197-204.
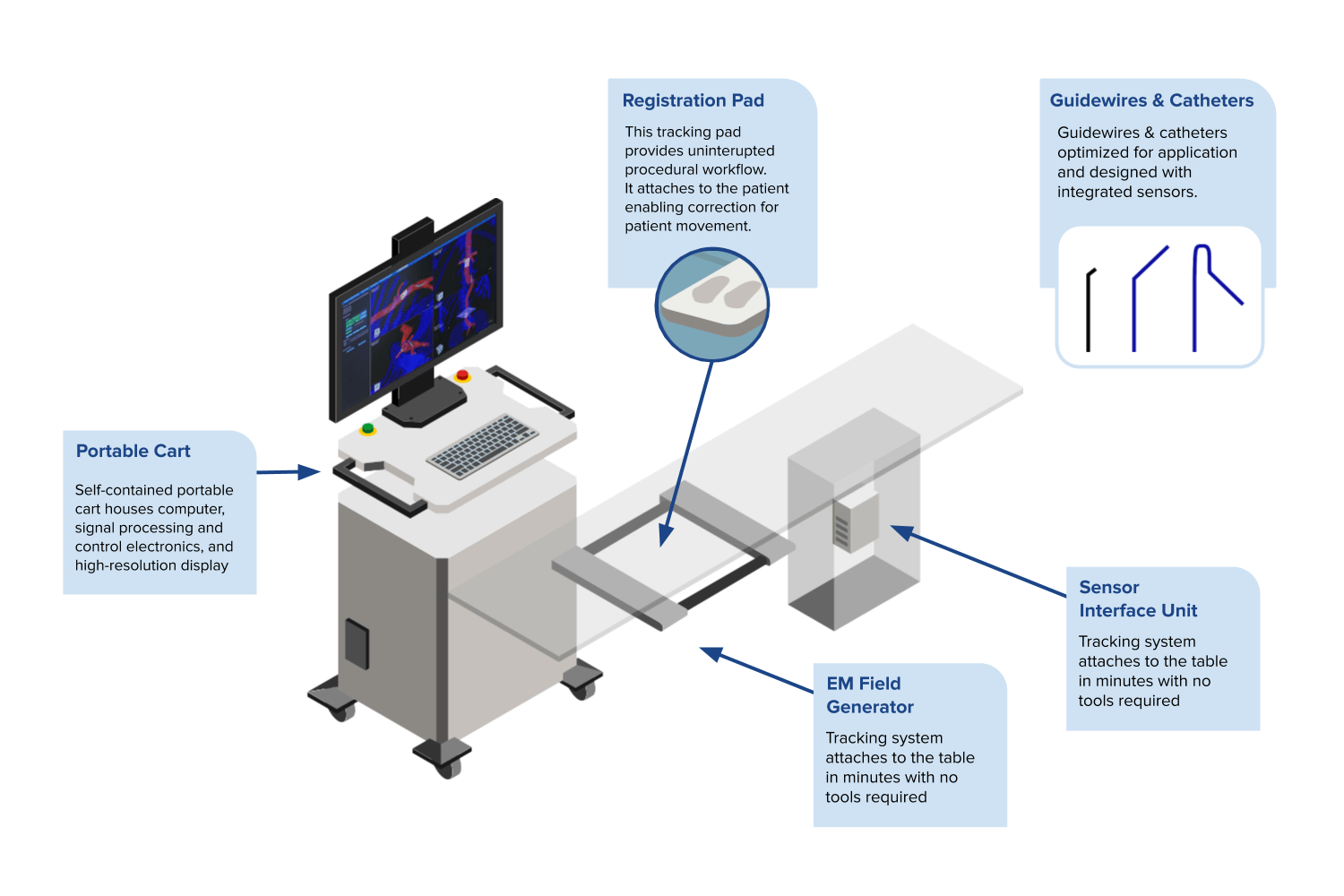
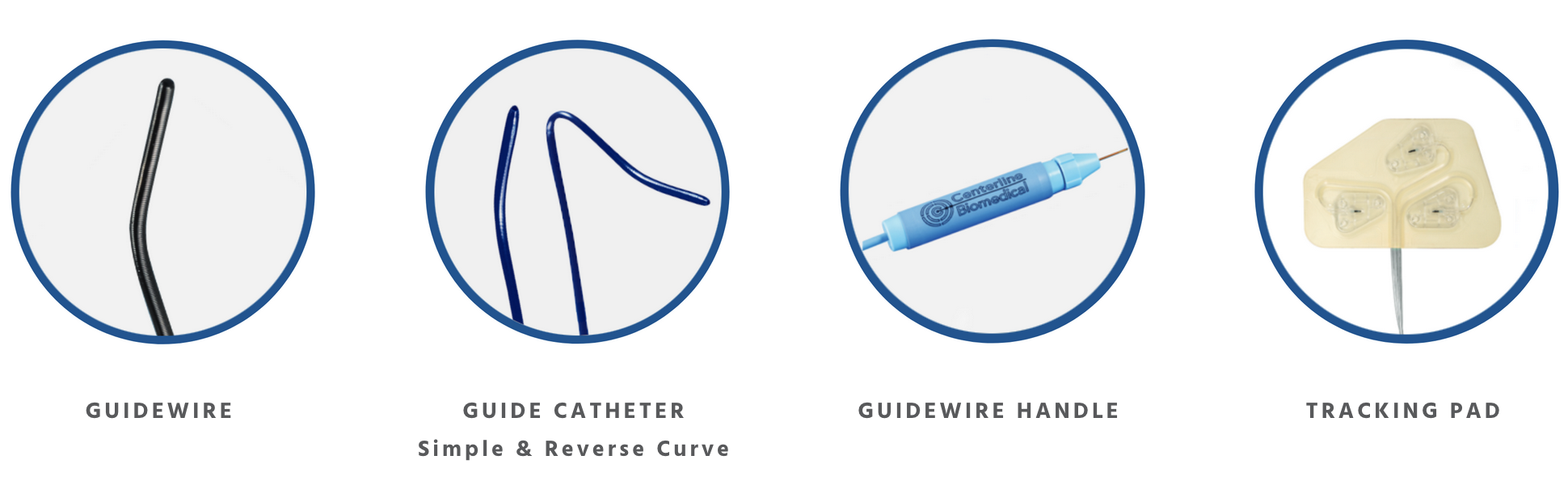
IOPS® Components
“Compared to standard imaging, we cut the procedural time by more than half during a preclinical study. Especially in complex interventions, every minute counts, and this should translate to the ability to treat more patients at less cost, with a simultaneous increase in precision safety.”