Endovascular surgery is an innovative, less invasive procedure used to treat problems affecting blood vessels. While this type of procedure has multiple benefits, they are also accompanied by several risks and complications to not only to patients but also to the physician and staff in the operating room. Below are a few key statistics that highlight some of these risks associated with this procedure.
Dangers of Prolonged Operating Time
Complications approximately doubled when operative time thresholds exceed 2 or more hours
Pooled analyses showed that the likelihood of complications increased significantly with prolonged operative duration, approximately doubling with operative time thresholds exceeding 2 or more hours.
Source: Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018 Sep;229:134-144. doi: 10.1016/j.jss.2018.03.022. Epub 2018 Apr 24. PMID: 29936980.
%
Complications increased by 14% for every 30 minutes of additional operating time.
Meta-analyses also demonstrated a 14% increase in the likelihood of complications for every 30 minutes of additional operating time.
Operational Costs in relation to Poor Patient Outcomes
%
Over 50% of these cases are the result of contrast exposure during cardiac catheterization
AKI Associated with Endovascular Procedures
Contrast administration during endovascular diagnostic or therapeutic procedures is one of the major causes of AKI and the third leading cause of hospital acquired renal failure in the US. Over 50% of these cases are the result of contrast exposure during cardiac catheterization, this number does not include post-contrast AKI following angiography or endovascular interventions for peripheral artery disease.
Increased Hospitalization Costs Due to AKI
AKI Associated with Endovascular Procedures
AKI was associated with an increase in hospitalization costs of $7933 (95% confidence interval [CI], $7608-$8258) and an increase in LOS of 3.2 (95% CI, 3.2-3.3) days compared to patients without AKI.
%
Vascular Surgery Readmission Rates
Cost of Readmissions after Common Vascular Procedures
Vascular surgery readmissions occur at a rate of 17% at 30 days and 27% at 90 days. Over half of the readmissions (55%) included at least one operation.
Source: Orr NT, El-Maraghi S, Korosec RL, Davenport DL, Xenos ES. Cost analysis of vascular readmissions after common vascular procedures. J Vasc Surg. 2015 Nov;62(5):1281-7.e1. doi: 10.1016/j.jvs.2015.05.037. Epub 2015 Aug 4. PMID: 26251167.
Readmission costs varied by reason with the highest costs occurring in readmissions for endoleaks
Cost of Readmissions after Common Vascular Procedures
Readmission costs varied by reason with the highest costs occurring in readmissions for endoleaks ($23,600), graft occlusion (median, $17,700) and renal insufficiency or failure (median, $15,000).
Source: Orr NT, El-Maraghi S, Korosec RL, Davenport DL, Xenos ES. Cost analysis of vascular readmissions after common vascular procedures. J Vasc Surg. 2015 Nov;62(5):1281-7.e1. doi: 10.1016/j.jvs.2015.05.037. Epub 2015 Aug 4. PMID: 26251167.
Interventionist’s Risks of Radiation Exposure to the Head
%
Approximately 85% of brain tumors from interventionists were on the left-side
Approximately 85% of brain tumors from interventionists were on the left-side, where there is a great radiation exposure. Tumors included glioblastoma multiforme, astrocytoma and meningiomas with a latency period of 12 to 32 years
%
Testing of eye doses underneath lead glasses during interventional procedures showed only 10-15% reduction in dose
Testing of eye doses underneath lead glasses during interventional procedures showed only 10-15% reduction in dose when compared to the dose just outside the glasses. These results, as well as others, indicate a wide variation in protection levels depending on the design of the glasses as well as individual behavior such as head orientation and positioning during fluoroscopy.
Shortcomings of Radiation Protection Equipment
%
Even more protection should be considered during high dose procedures and when treating high BMI patients (5.2% increase in exposure per unit BMI)
%
Lead is a potent neurotoxin, and 63% of lead aprons had lead dust on the outside of the aprons, some at significant levels
Unfortunately, lead inside the PPE’s does not always stay inside. Lead dust can come out the needle holes and cracks in the material.
Hazards of Career Exposure and the Long Term Effects
Head exposure equivalent to 50,000 chest x-rays across a 20 year interventional cardiology career.
Interventional cardiologists have the highest radiation exposure of any medical professional.
Career exposure:
(average 20 year interventional cardiology career)
– Head exposure equivalent to 50,000 chest x-rays
– Lower body exposure equivalent to 5,000 chest x-rays
Source: ORSIF
Exposed staff experienced a 2x increase of DNA damage
Source: Andreassi MG, Cioppa A, Botto N, Joksic G, Manfredi S, Federici C, Ostojic M, Rubino P, Picano E. Somatic DNA damage in interventional cardiologists: a case-control study. FASEB J. 2005 Jun;19(8):998-9. doi: 10.1096/fj.04-3287fje. Epub 2005 Mar 31. PMID: 15802491.
Exposed staff experienced a 6x higher rate of self-described anxiety/depression
Exposed staff members also experienced a 6× higher rate of self-described anxiety/depression
How can you mitigate these risks?
Advancements in navigation technology, such as Centerline Biomedical’s IOPS©, provide tangible mitigation opportunities for patients and caregivers by focusing on three key improvements.
IOPS© ADVANTAGES
Time Reduction
A recent in vitro study found that, overall, the mean time necessary to cannulate a given vessel using 3D navigation was 53.4% of the time necessary using traditional 2D navigation, indicating a time savings of 46.6%
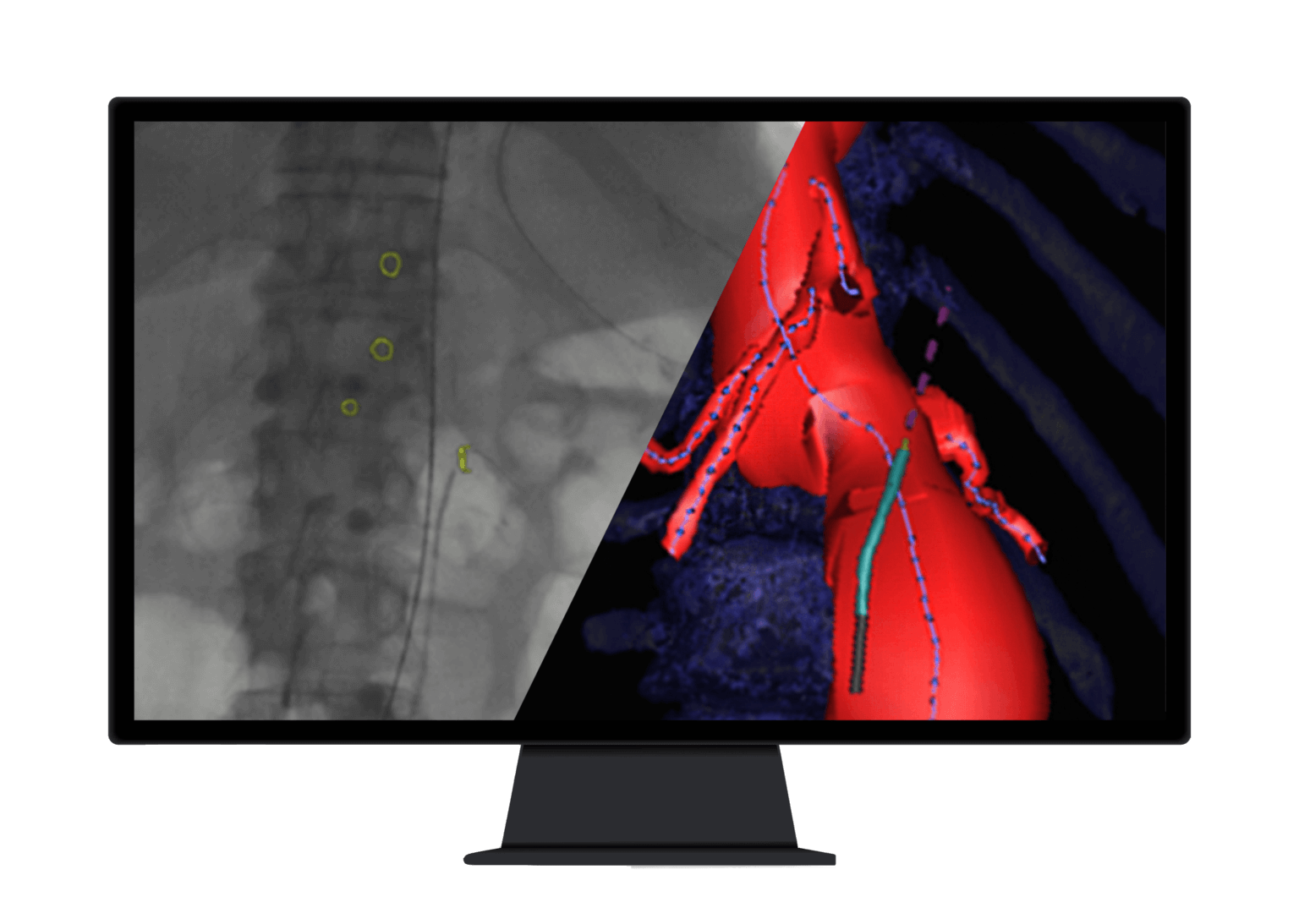
Patient outcomes are improved as we reduce procedural times with better visualization, greater control, and real-time position navigation data.
Mitigate the Growing Risk of Radiation Exposure and Contrast Dye
As endovascular procedures become more complex, the risk of radiation exposure continues to increase.